Nursing Best Practices for Social Media
Let’s look at the pros and cons of social media for nurses, and how we can successfully navigate the complexities and legalities of personal and professional life.
Our relentless research goes beyond shoes. Capsol allows us to talk all things nursing, from career advice and current news to self-care and mental health. These conversations with you, the community, and the world at large help us put our best foot forward when creating the best nursing shoes on the planet.

Though that doesn’t mean we just shouldn’t do it, or worse- be lazy about it. That begs the question of: Why is accurate and detailed charting so important?
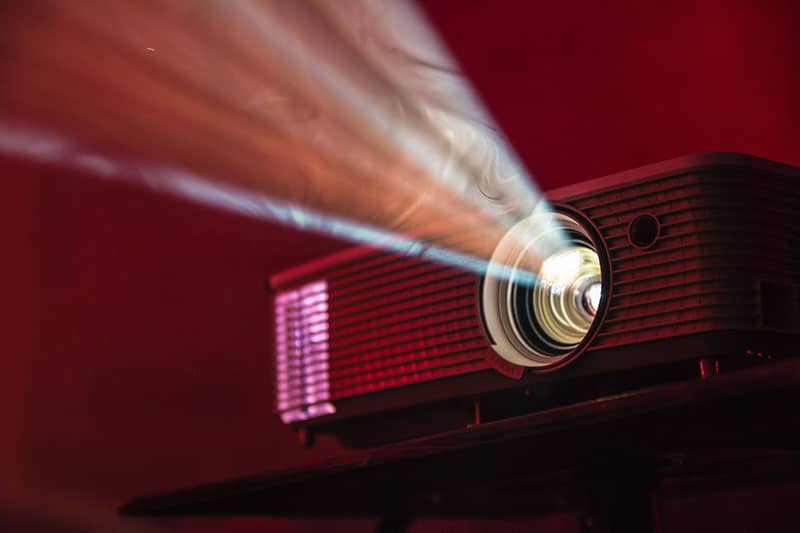
Well, a wise charge nurse once gave a good image. She said, “imagine everything you contribute into that patient’s chart on a giant projector screen in a courtroom”.
If that same documentation stood between you and no longer being a nurse, would you be cringing or would you be confident?
That documentation is what protects your license. We worked really hard for it, so we should be doing everything we can to protect it.
Not to mention that the nurse coming on after you, would love to be able to competently take care of the patient using their chart to have all the knowledge they need to succeed.
All of these things start with charting accurately and in detail!
But don’t worry, let’s break it down and make it easy!
Example: Patient A’s heart rate went into the 130’s around 0930, just after you have come on shift. Document the heart rate and the time. Then…
Example: I assessed Patient A, obtained up to date vital signs, observed for hemodynamic changes (and specify- shortness of breath, etc.) or asymptomatic, and called the physician who gave instruction to administer a beta-blocker. Document your assessment, up to date vital, medication administration, and the physician’s phone call including the exact date, time, and what was said.
Example: After medication administration, I obtained up to date vital signs which included a heart rate of 96 and assessed Patient A to make sure they were no longer having any symptoms. Document the assessment, up to date vital signs and resolution.
There you have it. Now if that episode ever comes into question, your license is covered. The next nurse now has the resources to accurately care for their patient. As a bonus, you earn respect from the physician for accurate and detailed charting! Its a win-win-win!
Now you can go home knowing that your patients are well taken care of. At the end of the day, that is why we became nurses, isn’t it?
Do you have any charting tips or tricks? Let the Capsol community on
https://www.nso.com/Learning/Artifacts/Articles/Do-s-and-Don-ts-of-Documentation
http://www.hpso.com/risk-education/individuals/articles/Documentation-Dos-and-Donts
Author
most recent
Let’s look at the pros and cons of social media for nurses, and how we can successfully navigate the complexities and legalities of personal and professional life.
Perhaps it’s a college application, professional resume, or something else. You want to volunteer. But where should you start? Here are a few…
This post explores why suicide among nurses has become a problem and what we can do about it. It’s a must-read for every nurse and anyone who knows a nurse.
0 Comments